-
Drancunculiasis카테고리 없음 2020. 3. 25. 16:34
Warning: This online archive of the CDC Prevention Guidelines Database is being maintained for historical purposes, and has had no new entries since October 1998. To find more recent guidelines, please visit the following:. at. at Strategies for Dracunculiasis Eradication D.R. Ruiz-Tiben Bulletin of the World Health Organization, 69(5): 533-540 (1991) WHO Collaborating Center for Research, Training & Eradication of Dracunculiasis and Guinea Worm Task Force, Div of Parasitic Dise NCID/Centerts for Disease Control & Prevention Reprint No.5205 Publication date: Table of Contents Tables Figures Strategies for dracunculiasis eradication D.R.
Hopkins. & E. Ruiz-Tiben. In 1991 the Forty-fourth World Health Assembly declared the goal of eradicating dracunculiasis (guinea worm disease) by the end of 1995. This article summarizes the recommended strategies for surveillance and interventions in national dracunculiasis eradication programmes. It is based on personal experience with dracunculiasis programmes in Ghana, Nigeria and Pakistan.
Three phases are described: establishment of a national programme office and conduct of a baseline survey; implementation of interventions; and case containment. The relevance of dracunculiasis eradication activities to strengthening of primary health care in the three countries is discussed briefly. Similar strategies would help eradicate this disease in the remaining endemic countries.
Introduction In May 1991 the Forty-fourth World Health Assembly endorsed the goal of eradicating dracunculiasis (guinea worm disease) by the end of 1995 (resolution WHA44.5). In 1988, the WHO Regional Committee for Africa had set itself the goal of eradicating the disease in all 17 remaining endemic African countries (except Sudan which is in the WHO Eastern Mediterranean Region) by 1995 (resolution AFR/RC38/R13). India and Pakistan are the two other countries still with this disease, which is only transmitted to humans when they drink contaminated water from stagnant ponds, cisterns or step wells. Eradication of dracunculiasis is feasible for the following reasons: there is no human carrier state beyond the one-year incubation period; there is no known animal reservoir; transmission is seasonal; active detection of individuals with worms protruding from skin lesions is a sensitive means of assessing the presence of the disease in villages; the methods for controlling transmission are simple and can be targeted effectively; and the total estimated cost of global eradication (about US$ 75 million) is moderate (1). Beginning in 1986, 1987, and 1988, the Global 2000 Project of the Carter Presidential Center assisted dracunculiasis eradication programmes in Pakistan, Ghana, and Nigeria, respectively, in collaboration with the ministries of health of those countries.
The WHO Collaborating Center for Research, Training, and Eradication of Dracunculiasis at the Centers for Disease Control also provided extensive technical consultation to these programmes. This paper summarizes the strategies for eradicating dracunculiasis, based mainly on our experiences to date in Pakistan, Ghana and Nigeria. We believe a description of these strategies can help other countries that are just beginning their eradication programmes or are on the verge of eliminating the disease. This is particularly important now that most of the remaining endemic countries are initiating national programmes as a part of the global effort to eradicate dracunculiasis by 1995 (2). The principles of the eradication strategy are common to all programmes, though they must be adapted to the epidemiological circumstances and resources of each endemic country (3). Helping the affected villagers to help themselves should be the guiding philosophy of the programme.
Residents of endemic villages have been found to be the most motivated to get rid of guinea worms because they appreciate the improvement in their own lives and other benefits resulting from the elimination of this disease. Priority should be given to those endemic villages or areas that manifest the most willingness to help themselves. The fundamental difference between an eradication programme and a control programme is critical to understanding the need for some of the strategies recommended in this paper.
While a control programme may aim to reduce the incidence of a disease until the disease is no longer a public health problem, an eradication programme has a more demanding and specific objective: to reduce the incidence of the disease to zero within a given time period. Control efforts may be limited to areas of moderate or intense transmission, whereas eradication programmes must encompass all areas where transmission occurs, including areas of low incidence. An eradication programme has a fixed endpoint and a limited duration of expenditures, but control programmes and their costs continue indefinitely. Finally, the need for extremely sensitive surveillance to detect all cases, including imported cases, wherever they may occur in the at-risk area, is much more critical in an eradication programme, whereas a control programme may be adequately served by sampling or sentinel surveillance measures. Strategies The key necessary activities of dracunculiasis eradication programmes may be grouped into three operational phases. Phase I: establishing a national programme office and conducting baseline surveys Each endemic country must designate a national programme coordinator, and establish a small staff/secretariat to support the leadership and coordination roles of the national office of the eradication programme.
The two most critical first tasks of this office, if they have not been done already, are to conduct a nationwide, village-by-village survey, and prepare a national plan of action for eradicating dracunculiasis from the country. The main priority of the national survey should be to identify all endemic villages in the country, and secondly to count the number of annual cases of the disease, so as to establish the true extent of the problem (3). The national survey provides an important basis for preparing or revising a plan of action that reflects the true scope of the national problem. The plan of action provides the basis for mobilizing the necessary national and external support. Countries where the disease occurs nationwide may find it necessary to develop plans of action for each endemic state or region. In most instances, it will be advisable for the programme to also establish, or make use of an existing intersectoral committee or national task force in order to facilitate mobilization and coordination of the diverse governmental and other agencies whose contributions are needed, such as the government ministries concerned with health, water supplies, and information.
National secretariats in support of the national eradication programmes, including one expatriate adviser, were established in the respective ministries of health with the assistance of Global 2000 in Pakistan (in 1987), Ghana (1987) and Nigeria (1988). Draft plans of action were prepared, and then modified accordingly after the first national survey was completed in each country. Target dates for eliminating the disease were set at 1990 for Pakistan, 1993 for Ghana, and 1995 for Nigeria. Of the three, only Nigeria established a national task force for guinea worm eradication (in 1988) which meets quarterly. By the end of 1988, each of Nigeria's 21 states and the Federal Capital Territory had established comparable intersectoral state task forces, beginning with Anambra State in 1986. The eradication programme in Pakistan conducted a national village-by-village search for cases from April to June 1987. It found that 408 villages had been affected by the disease in the past three years, with an estimated 2400 cases occurring in the previous one year, which was much less than had been expected, based on passive reporting.
Nigeria conducted two nationwide surveys, in 1988-89 (August-March), and 1989-90 (December-March), followed by a survey of known endemic areas only in 1990-91 (November-February). Approximately 640 000 to 650 000 cases were enumerated in 6000 Nigerian villages during the first two searches.
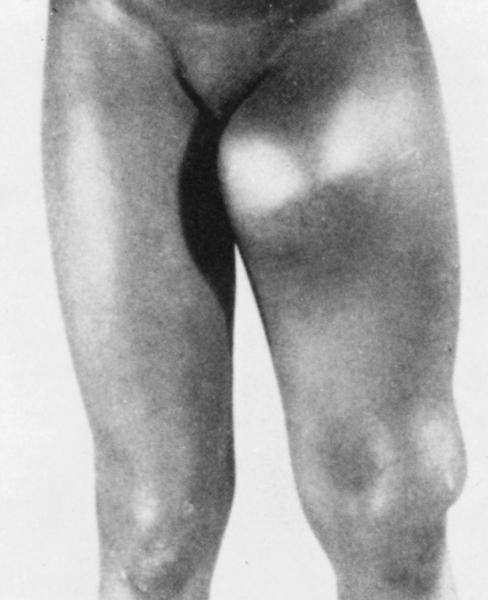
Dracunculiasis Symptoms
Ghana conducted a national search for cases in 1989-90 (November-January), and found that almost 180 000 cases had occurred in the past year in about 6500 villages. Previously, the annual reports of dracunculiasis in Ghana and Nigeria had totalled less than 5000 cases per country. Post-search evaluations of varying intensity were conducted after each of these national surveys. Phase II: implementing interventions Active surveillance is also the key to implementing interventions, monitoring progress, and evaluating the impact of the programme, just as it is to planning the attack and mobilizing the necessary resources (3).
A vertically organized, quickly conducted national search is the best means of ascertaining the extent of the disease at the outset. In the next phases of the programme it is very desirable to rely on village-based workers, one or more in each known endemic village, to maintain village-based case registers and provide monthly reports of cases as they occur.
The advantages of the latter system are that it provides more accurate surveillance, allows monthly tracking of incidence, is compatible with the primary health care (PHC) system to which most countries are already committed, eliminates the need for annual mobilization of active case searches, and provides the documentation of programme impact needed for verifying the absence of transmission, i.e., the attainment of eradication. Identification and training of village-based workers in each of the known endemic villages is perhaps the most urgent early task of the intervention phase. Where they exist already, primary health care (PHC) workers in endemic villages should be used; where they do not yet exist, an appropriate villager should be designated (who may later be incorporated into the country's PHC programme). In addition to their roles in reporting cases of dracunculiasis monthly, the village-based workers can also be trained to provide health education about the disease to their neighbours, and provide simple topical treatment of wounds caused by the emerging worms. Apart from training, a system for providing regular supervision and supplies for the village-based workers must be established if one does not already exist. The issue of whether such workers are to be volunteers, or paid by the village, or compensated by the programme must be decided by each national authority. Following the search for cases in 1987, the guinea worm eradication programme (GWEP) in Pakistan instituted its ongoing active surveillance and control activity by identifying and training one village implementer (VI) in each of the approximately 400 recently endemic villages.
These VIs were each paid about 200 rupees (about US$ 10) per month by the GWEP to maintain case registries and report cases monthly. After an end-of-year evaluation in 1988, a tier of sector supervisors was trained, one for up to 20 VIs, to improve supervision of the VIs under the guidance of the previously established regional manager for each of the three endemic provinces. The programme in Ghana began identifying and training a resident volunteer to report cases of dracunculiasis in each endemic village early in 1989, but had to interrupt this system in order to conduct its nationwide search for cases starting in October that year. It reverted to monthly reporting by volunteers in endemic villages later in 1990. Nigeria depended on annual national searches for cases to track the incidence of dracunculiasis in 1988-90, similar to the model of biannual active searches used until recently in the Indian GWEP (4). The third Nigerian survey in 1990-91 covered the known endemic local government areas only, and included intervention measures, after which that programme began converting to village-based monthly reporting, using primary health care workers where available. Each endemic country must also decide on the most appropriate mix of the available interventions (health education, provision of rural water supply, use of cloth filters, and vector control) that it can afford or should seek external help for this.
No single intervention will work everywhere. 'Problem' villages can be dealt with as they become apparent.
After most or all of the endemic villages have been identified through the national survey, the goal should be to get interventions started in all these villages as fast as possible. Establishing and training the village-based workers to implement active surveillance and control are probably the first step in such interventions, which should include the following. Health education and community mobilization should be emphasized as a priority because they are the least costly of the interventions available, and are a necessary base for the other interventions. Each country needs to devise an overall plan and comprehensive strategy for health education and community mobilization, taking into account the relevant characteristics and resources of the country and its population. The goal here should be to get the same basic messages to endemic populations repeatedly, using all appropriate channels. The three essential messages are:. guinea worms come from drinking contaminated water;.
persons with emerging worms or blisters should not contaminate sources of drinking water;. people can also protect themselves by always filtering or boiling their drinking water, or by only drinking water from safe sources. The village-based worker, a key source (but not the only one) for the health education messages, should be reinforced by religious and traditional/political leaders in the village, schoolteachers, agricultural and other extension workers, community organizations, and by the mass media (radio, posters, etc.) in the local languages. These activities will create a demand for cloth filters (which can be distributed and their proper use demonstrated by the village-based workers), as well as mobilize support for local participation in the other interventions (water supply, control of copepods). The logistical system should be prepared to meet the increased demand for cloth filters by providing timely supplies to the village-based workers.
Provision of a safe source of drinking water, such as a bore-hole well with handpump, or a properly constructed hand-dug well, is the other priority intervention. This is the most desirable intervention, since it yields many other important benefits besides eliminating dracunculiasis. But this is also the most expensive of the interventions, especially in smaller communities, and the geological features may not permit this to be used in some affected areas. The overall goal of the eradication programme should be to try to get safe wells provided or rehabilitated in as many of the identified endemic villages as possible and as quickly as possible, especially in the most highly-endemic, densely-populated areas.
Among priority areas with the latter characteristics, the highest priority might be given to localities with the greatest agricultural potential. The programme should seek to get a decision by the government to provide safe water to the endemic villages as a national priority, since such villages are usually the worst off of all the unserved villages. These populations are suffering from dracunculiasis, with its adverse effects on health, agriculture, and school attendance, in addition to the other negative effects of unsafe water that all unserved villages have in common.
The villages with dracunculiasis are also only a small fraction of all such unserved villages. Other appropriate technologies such as rainwater harvesting, conversion of step wells into draw wells, or construction of small sand filters, for example, should also be considered, and used where appropriate and necessary. The control of copepod populations using Abate. (temephos) is intermediate in cost, relative to the promotion of health education or use of cloth filters and rural water supplies. It should be used only in selected endemic villages, as backup to health education and/or water supply interventions.
It should be considered for use in 'epidemic control' in very highly affected villages with limited drinking-water sources, to reduce the incidence (while villages wait for a safe water source to be installed) in situations where compliance with health education is poor or where providing a safe water source is not feasible, or to provide a second or third barrier to transmission for additional security in areas where dracunculiasis elimination is imminent or was recently achieved. This intervention is not cost-effective when the volume of the drinking-water source exceeds 500 cubic metres. The programme in Pakistan has from its inception relied exclusively on health education, use of cloth filters, and temephos to eradicate dracunculiasis, mainly because many residents strongly prefer water from ponds or cisterns, compared to underground water which in many of the endemic areas is brackish. Village implementers are the main providers of health education on dracunculiasis prevention, and they also distribute the cloth filters and monitor their use. Field workers from local health departments were trained by the GWEP to apply temephos. Ghana and Nigeria began conducting extensive systematic interventions in endemic villages in 1990, although in Nigeria the UNICEF-assisted rural water supply programmes had been giving priority to endemic villages since 1984, and Anambra State had begun health education and community mobilization activities in 1986. Apart from India, so far only Nigeria has established a national policy of priority to endemic villages for sources of safe drinking water (in 1989).
Dracunculiasis Removal
In Ghana, the head of state visited 21 villages in 1988 to demonstrate personally the use of cloth filters. Ghana also began distributing tens of thousands of copies of a manual to secondary schools in 1989 for teaching about dracunculiasis. Both Ghana and Nigeria are emphasizing health education, community mobilization, and rural water supply in their interventions so far; more extensive use of temephos in selected villages will be carried out in 1991.
A schematic illustration of the extension of recommended intervention measures is given in, where the unit of consideration is the endemic village. Whatever the number of endemic villages at the beginning of a programme, towards the end all the residual endemic villages should be included in the case-containment strategy. An appropriately organized and implemented dracunculiasis eradication programme should be able to mobilize sufficient resources to eliminate all indigenous transmission within five years after the first national case search is conducted. In some countries, it may be appropriate to begin using temephos sooner than indicated in, provided the two priority interventions of health education/cloth filters and water supply are already being implemented. The key activities needed in national dracunculiasis eradication programmes are summarized in.
Phase III: case containment As programmes get closer to achieving eradication, i.e., when the expected case load of the village-based health worker is one (or less than one) case per worker per day, increasingly stringent surveillance and control measures will be indicated, particularly if transmission is unlikely to be re-established as a result of introduction of infections from other endemic areas. Of the three programmes assisted by Global 2000, only Pakistan has reached this stage, although some less endemic areas of Ghana and Nigeria will begin implementing this strategy in 1991. As applied in the GWEP in Pakistan, this strategy is additive, providing for rapid attention to each case of the disease, not just to the endemic villages.
The village-based workers, being the best means for immediate detection of new cases, are essential to this stage of the programme, and for preventing any further transmission from them. In addition to educating the afflicted individual not to contaminate drinking-water sources and making sure that other inhabitants of the village are aware of the case and have cloth filters to protect themselves (if necessary), the trained village worker can try to determine whether the patient may have already contaminated a source of drinking water, and also where the patient acquired the infection the year before.
Providing simple medical treatment to patients becomes much more important and feasible at this final stage of the programme. If the resources are available, simple topical treatment should be provided from the outset of the eradication programme, but not if it detracts from providing the other more effective interventions to prevent new infections. Provision of treatment free of charge is a useful incentive for patients to contact the health service, where they can be educated about the disease and where their case can be recorded.
The case-containment strategy has been applied in Pakistan from the beginning of 1990 (6); orientation to the new strategy began in February, two months before the onset of the transmission season. Key elements of this strategy, compared to the previous strategy in Pakistan, were the use of new case investigation forms for VIs and sector supervisors, which ensured that all the appropriate questions were asked and all the prescribed control measures were carried out, whenever a case occurred, and use of revised performance criteria to encourage and monitor the promptness with which these measures were taken. By the end of August 1990, when a cumulative total of 121 cases had been reported, data for 99 of them revealed that 87.9% of the cases were confirmed and containment measures initiated by the VI within one day of worm emergence. Sector supervisors had confirmed 63% of the cases within one day, and 88% of the cases within four days of worm emergence. Regional managers visited 82% of the cases within one week.
In Pakistan, the rates of decline in incidence of dracunculiasis exceeded 50% each year during the first two years, from approximately 2400 cases in 1987 to 1110 in 1988, and 534 in 1989. The rate of decline from 1989 levels to 1990 (160 cases) was about 70%, suggesting significantly increased effectiveness under the new strategy. The epidemiological results of the case-containment strategy implemented in 1990 will be manifest in 1991, when it is expected that Pakistan will probably have no more indigenous cases of dracunculiasis. WHO will expect recently endemic countries to maintain adequate surveillance for at least three years following the last indigenous case, so that they may qualify for certification of elimination.
Thus surveillance is also the key to documenting the eradication process. Discussion The critical importance of the first national active search for cases, village-by-village, cannot be overemphasized.
The search results were surprising in all three countries. In Pakistan, there was significantly less disease than had been expected on the basis of passive reporting. In Nigeria and Ghana, there were far more cases than most authorities expected, although in Nigeria some earlier projections of actual incidence were more than twice the documented incidence. The results of these searches were the basis for realistic national plans of action, and for mobilizing the necessary support of governmental and other leaders. There is no substitute for conducting at least one active search for cases nationwide in each endemic country. Some early examples of the contributions of these three programmes to the strengthening of primary health care activities in the countries concerned should also be noted, given the present concern about 'vertical' programmes that focus on eradicating one disease.
For example, in Pakistan, a trained network of village implementers, who are accustomed to supervision and are obviously capable of reporting every month some other diseases and providing simple topical treatment of wounds, is available in over 500 formerly endemic villages. In Nigeria, vaccinators for the expanded programme on immunization conducted immunizations in villages they had never before visited, in the course of accompanying guinea worm search teams during the third survey in 1990. In Ghana, the searchers inquiring about dracunculiasis asked also about presence of haematuria during their visits to virtually all villages in the country, and thereby compiled the first village-specific data about the distribution of schistosomiasis haematobium in Ghana at the same time. The health education and community mobilization components of the dracunculiasis eradication programmes, and their stimulation of participating public health workers are among the other positive long-term benefits that can be expected.
The effectiveness of the measures used in Pakistan are already evident. India, which began its eradication programme in 1980, and counted nearly 45 000 cases in 1983, had reduced its annual cases by over 90%, to under 4000 cases, by 1990 (Dr Ashok Kumar, personal communication, 1990). With the adoption of more intensive containment measures, it is expected that India, which up to now had had annual rates of decline of about 30%, will soon eliminate the disease from the only remaining endemic area in Asia. The main focus of attention for dracunculiasis eradication must now be on Africa, where national ministers of health, meeting under the auspices of the WHO Regional Office for Africa (including all affected African countries except Sudan, a member of WHO's Eastern Mediterranean Region), resolved in 1988 to eradicate dracunculiasis by the end of 1995. In eastern Africa, Global 2000 began assisting a national dracunculiasis eradication programme in Uganda in 1991, and Kenya appears to have only a minor focus of infection in the adjoining Turkana District. Only limited control measures are now possible in Sudan and Ethiopia, the only other endemic countries in East Africa, owing to the civil unrest in both countries. Much more could be done now in francophone West Africa, which must mobilize fully in 1991 if it is to eradicate dracunculiasis by 1995.
UNICEF agreed to assist and fund the national searches for cases, starting in 1989, in the other endemic African countries besides Ghana and Nigeria. Dupont de Nemours & Co. And Precision Fabrics Group, and the American Cyanamid Company have donated ample supplies of nylon filter material and Abate, respectively, for the national programmes in Africa. Other donors are also prepared to help countries that organize themselves with the intention of eradicating this disease.
Appropriate adaptation of the strategies described here will help the remaining endemic countries to eradicate dracunculiasis. Ghana and Nigeria each reduced the incidence of dracunculiasis by over 30% between 1989 and 1990 (7).
Acknowledgements Funding for the assistance by Global 2000 was provided by the Bank of Credit and Commerce International until early in 1990; since then by His Highness Shaikh Zayed bin Sultan Al Nahyan, President of the United Arab Emirates. The programme in Pakistan has been and is funded separately, by the Bank of Credit and Commerce International Foundation. The United States Agency for International Development (USAID) mission to Ghana provides significant additional support for the programme in that country, while the UNICEF mission to Nigeria and the government of Japan provide substantial support to the Nigerian programme. References. Centers for Disease Control. International Task Force for Disease Eradication.
Morbidity and mortality weekly report, 39:209-212 (1990). Hopkins, D.R.
& Ruiz-Tiben, E. Dracunculiasis eradication: target 1995.
American journal of tropical medicine and hygiene, 43:296-300 (1990). Guinea worm disease: epidemiology, control and treatment. Bulletin of the World Health Organization, 57:683-689 (1979). Richards, F. & Hopkins, D.R. Surveillance: the foundation for control and elimination of dracunculiasis in Africa.
International journal of epidemiology, 18:934-943 (1989). Dracunculiasis - India. Weekly epidemiological record, 64:159-162 (1989). Centers for Disease Control. Update: dracunculiasis eradication - Pakistan, 1990.
Morbidity and mortality weekly report, 40:5-7 (1991). Centers for Disease Control. Update: dracunculiasis eradication - Ghana and Nigeria, 1990. Morbidity and mortality weekly report, 40:245-247 (1991).
Senior Consultant, Global 2000, Carter Center, Inc., Atlanta, GA, USA. Coordinator, Guinea Worm Task Force. Division of Parasitic Diseases (F22), CID, Centers for Disease Control, Atlanta, GA 30333, USA (requests for reprints should be sent to this address), and WHO Collaborating Center for Research, Training and Eradication of Dracunculiasis.
5205. Use of trade name is for identification only and does not imply endorsement by the Public Health Service or the U.S. Department of Health and Human Services. POINT OF CONTACT FOR THIS DOCUMENT: To request a copy of this document or for questions concerning this document, please contact the person or office listed below.
If requesting a document, please specify the complete name of the document as well as the address to which you would like it mailed. Note that if a name is listed with the address below, you may wish to contact this person via CDC WONDER/PC e-mail. DIVISION OF PARASITIC DISEASES CDC/NCID/DPD MS F-22 1600 Clifton Rd.